BMI Sidelined in New Obesity Definition That Favors Health Evaluation
Table of Contents
Introduction
Why BMI Falls Short
The New Approach to Defining Obesity
Preclinical Obesity
Clinical Obesity
Global Impact of Obesity
New Diagnostic Methods
Importance of Personalized Assessments
Addressing Stigma in Obesity Care
Conclusion
Introduction

A group of 58 researchers has proposed a groundbreaking redefinition of obesity, moving away from the long-standing reliance on Body Mass Index (BMI). Published on January 14, 2025, in The Lancet Diabetes & Endocrinology, this updated framework emphasizes assessing the impact of excess body fat—also called adiposity—on overall health, rather than solely focusing on weight and height ratios. This shift could significantly enhance clinical care, public health policies, and societal attitudes toward obesity.
Why BMI Falls Short
BMI, which links a person’s weight to their height, has been the primary tool for diagnosing obesity due to its simplicity. However, it fails to account for:
- Differences in body composition (e.g., muscle vs. fat).
- Ethnic and gender-based variations in health risks.
- The nuanced effects of excess body fat on organ function.
For example, a muscular athlete might be misclassified as obese, while someone with a “normal” BMI could still have harmful levels of body fat.
The New Approach to Defining Obesity
The proposed redefinition categorizes obesity into two main types:
Preclinical Obesity
- Definition: Excess body fat without significant damage to organs or tissues.
- Risk: Higher risk of developing health issues compared to individuals without obesity.
- Treatment: Preventative measures such as counseling and lifestyle modifications.
Clinical Obesity
- Definition: Excess body fat causing harm to organs, tissues, or daily activities.
- Risk: Significant health complications, such as diabetes or cardiovascular diseases.
- Treatment: Requires targeted interventions, including medication, lifestyle changes, or surgery.
This nuanced framework ensures tailored care for individuals based on their specific health status.
Global Impact of Obesity
With over 1 billion people living with obesity worldwide, the condition contributes to approximately 5 million deaths annually. Conventional methods of diagnosis and treatment often:
- Over-treat individuals without significant health risks.
- Miss those who need medical intervention.
By redefining obesity, healthcare systems can allocate resources more effectively and address the condition’s complexity.
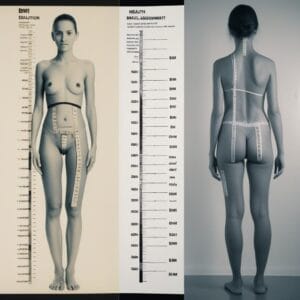
New Diagnostic Methods
The revised framework combines BMI with additional tools, including:
- Waist circumference: A proxy for adiposity.
- Body scans: Low-level X-rays to measure fat mass.
- Alternative markers: Waist-to-hip or waist-to-height ratios.
- Laboratory tests: Standard health checks to identify organ damage.
These methods provide a more comprehensive understanding of an individual’s health.
Table: Comparison of Diagnostic Tools
| Method | Advantages | Limitations |
|---|---|---|
| BMI | Simple and cost-effective | Lacks precision for individuals |
| Waist Circumference | Measures central fat distribution | May not account for muscle mass |
| Body Scans | Accurate fat mass measurement | High cost and limited access |
| Laboratory Tests | Assesses overall health impact | Requires specialized equipment |
Importance of Personalized Assessments
The researchers highlight the need for personalized obesity assessments, considering:
- Age: Older individuals might face different risks.
- Gender: Women and men store fat differently.
- Ethnicity: Some populations experience health risks at lower BMI thresholds.
Personalized diagnostics ensure more accurate and effective treatments for diverse populations.
Addressing Stigma in Obesity Care
Obesity is often misunderstood as a simple issue of willpower. However, factors such as hormonal changes, genetics, and societal pressures play significant roles. Stigma in healthcare settings prevents many individuals from seeking help, further exacerbating the problem. Improved education and communication are crucial to overcoming these challenges.
Key Quote
“If it were so simple as eating less and moving more, we wouldn’t have an obesity epidemic,” says Elisabeth van Rossum, an endocrinologist at Erasmus University Medical Center Rotterdam.
Conclusion
The redefined framework for diagnosing obesity represents a major step forward in understanding and managing the condition. By focusing on the health impacts of adiposity rather than solely on BMI, this approach offers a more accurate, equitable, and effective way to address the global obesity epidemic. Future clinical guidelines should incorporate these findings to ensure better health outcomes for individuals worldwide.
